Yes, physiotherapy can be very helpful for managing osteoarthritis (OA). While it cannot cure OA, physiotherapy can significantly improve quality of life and manage symptoms. Here’s how:
1. Pain Management:
Modalities like heat, cold therapy, or TENS (Transcutaneous Electrical Nerve Stimulation) can help reduce pain and inflammation, providing relief for those with OA. They can also give advice on exercise and activity modifications to make movements less painful.
2. Strengthening Exercises:
Strengthening the muscles surrounding the affected joint helps to stabilise and support the joint. This can reduce strain on the cartilage and decrease pain over time.
3. Range of Motion Exercises:
Physiotherapists can guide you through stretching and mobility exercises to maintain or improve the joint’s flexibility. This can help reduce stiffness and increase the range of motion.
4. Posture and Body Mechanics:
Physiotherapists can teach you how to adjust your posture and movement patterns to avoid putting additional strain on the affected joints, which can help in reducing pain and prevent further damage.
5. Weight Management:
If OA is in the weight-bearing joints (like the knees), physiotherapists may also work with you on strategies to reduce weight, as this can help reduce the load on the joints and alleviate symptoms.
6. Assistive Devices:
In some cases, a physiotherapist can recommend the use of assistive devices like braces, orthotics, or walking aids to support the affected joint and reduce pain during daily activities.
7. Education and Self-Management:
A physiotherapist can provide education on lifestyle modifications, including joint protection techniques, and ways to manage flare-ups of pain, allowing you to take control of your condition.
8. Aerobic Conditioning:
Gentle aerobic exercises (like walking, swimming, or cycling) can help improve cardiovascular health and overall stamina while avoiding high-impact stress on the joints.
In summary, physiotherapy focuses on reducing pain, improving movement, and preventing further deterioration, making it a key component of an overall management plan for osteoarthritis.
Here at Auckland Physiotherapy we are able to examine and diagnose your hip and knee condition and give you an individually tailored Arthritis care plan.
For more information, read about Arthritis Care at Auckland Physiotherapy or Mark Quinn's Blog on Arthritis Management. We also offer relief from arthritis packages.
For more information, come into our clinic (close to Remuera, Newmarket and Parnell) to speak to our expert team. It is essential you first get the right diagnosis before any treatment and management occur so book in for a first appointment.

Check out our Online Store for great Rehab and Health goods.


There are several common foot problems that people experience, and podiatry is a branch of medicine dedicated to diagnosing and treating these conditions. Here are some of the most common foot problems and how podiatry can help:
At Auckland Physiotherapy, our Podiatrist has been practising in musculoskeletal podiatry for 13 years and has studied for 9 years (so far…). He holds his Masters and is on track to finish his PhD in 2023. Meet Aaron Jackson here. To book an appointment, book online or call our team on 09 3664480.
Is that nagging neck pain affecting your daily life? You're not alone. Neck pain is one of the most common musculoskeletal conditions we treat. Let's explore effective strategies to manage and resolve your neck pain.
Understanding Neck Pain Common causes include:
Evidence-Based Treatment Approaches
Prevention Strategies Maintain good neck health by:
Recovery Timeline Most people experience improvement within:
Common Questions;
Mobilisations and massage can give you short term relief. For greater short- and long-term improvements in pain and quality of life, exercise combined with manual therapy give better results in comparison to manual therapy alone.
2. Do I need to see my GP before seeing a Physio?
No, you do not need to see your GP before seeing us at Auckland Physiotherapy. Our expert team can lodge your ACC claim and refer you for imaging and specialist reviews if required. Our Physiotherapists have a wealth of knowledge in assessing and diagnosing your pain. We believe this is the most important part of your recovery as once you know what is wrong, you can use the most evidenced based treatment specific for that condition.
3. Can Poor Posture cause neck pain?
Yes, absolutely. Poor posture, especially from sitting at a desk for long periods, looking down at a phone or hunching over can over time cause stress and strain to the muscles, ligaments and joints, leading to pain.
4. Is neck pain related to stress?
Yes, stress can cause muscle tension in the neck and shoulders, which can lead to pain and discomfort. It can also alter the way you breath which in turn makes you use your neck muscles to help you breath.
5. Can neck pain cause Headaches?
Yes, neck pain is often associated with tension headaches and migraines. The muscles around your neck and your upper neck joints can refer pain to your head. At Auckland Physio, we have a specialised Headache Clinic with our expert Masters Physio Robyn Atkinson, who works with people to overcome headaches. She uses the Evidenced-based Watson Approach.
6. Is neck pain common as we age?
Yes, neck pain tends to increase with age due to conditions like osteoarthritis or degenerative disc disease.
7. What can I do to prevent neck pain?
Regular exercise, maintaining good posture, good ergonomics and taking frequent breaks can help prevent neck pain. We suggest you see a Physiotherapist early to help instead of waiting.
For more information, come into our clinic (close to Remuera, Newmarket and Parnell) to speak to our expert team. It is essential you first get the right diagnosis before any treatment and management occur so book in for a first appointment.

Check out our Online Store for great Rehab and Health goods.


Frozen shoulder, or adhesive capsulitis, can be a frustrating and painful condition. This comprehensive guide will help you understand the condition and explore effective treatment options.
What is Frozen Shoulder? Frozen shoulder involves:
The Three Phases:
Treatment Approaches
Recovery Tips:
If you think you have a frozen shoulder, come to Auckland Physio, Parnell clinic to see one of our Physiotherapists. You can book easily online HERE or call our friendly reception team on 093664480. Alternatively, if you're not sure if Physio can help, book a Auckland Physio complimentary call.
Common Questions
Yes, Physiotherapy can be very effective in treating frozen shoulder (adhesive capsulitis). Physiotherapists use a combination of treatments to reduce pain, increase the range of motion, and improve function in the shoulder.
Common physiotherapy techniques at Auckland Physiotherapy include:
If you're dealing with frozen shoulder, it’s important to work closely with a physiotherapist who can guide you through exercises and treatments specific to your condition. It may take time, but physiotherapy can lead to significant improvement.
2. How long does it take for a Frozen Shoulder to go?
A frozen shoulder can be a slow and frustrating condition, and the recovery timeline can vary from person to person. Generally, it progresses through three stages:
1. Freezing stage (painful phase): This stage lasts 6 weeks to 9 months, where the shoulder becomes increasingly painful, especially with movement, and its range of motion starts to decrease.
2. Frozen stage (adhesive phase): This stage can last 4 to 6 months. The pain may decrease, but the shoulder becomes stiff, making it difficult to move. Function is limited.
3. Thawing stage (recovery phase): This can take anywhere from 6 months to 2 years. During this stage, the shoulder gradually regains mobility, and pain continues to decrease.
In total, recovery from a frozen shoulder can take anywhere from 1 to 3 years. Without treatment, spontaneous complete or nearly-complete recovery over a varied period of time occurs. However, with proper treatment, including physiotherapy, the recovery time can be shortened, and the condition can be managed more effectively. Regular stretching and strengthening exercises, along with professional guidance, can help speed up the recovery process and improve outcomes.
3. What causes frozen shoulder?
A Frozen Shoulder affects about 6% of the population. The exact cause is not fully understood, but it is often linked to shoulder injury, surgery, or conditions like diabetes, thyroid disorders, and heart disease. It can also occur without any apparent reason.
4. How do I know if I have a frozen shoulder?
Symptoms include pain and stiffness in the shoulder, difficulty moving the arm, especially in certain directions (like overhead or behind the back), a limited range of motion and pain sleeping on the affected side. At Auckland Physio, our expert Physio team will assess your shoulder and do a range of special tests to try and diagnose your pain. You may be asked to get an X-ray and Ultrasound to rule out any other injuries. You may also be referred to a specialist for further management.
5. Can frozen shoulder go away on its own?
Yes, but it can take a long time—sometimes up to 2 to 3 years. Treatment, like physiotherapy, can help speed up recovery and reduce pain.
6. Can physiotherapy cure frozen shoulder?
Physiotherapy can significantly help reduce pain, improve range of motion, and restore function, but full recovery can take time and may require a combination of treatments.
7. What are the risk factors for a Frozen Shoulder?
Common risk factors include age (typically 40-60 years old), diabetes, heart disease, recent shoulder surgery or injury, thyroid disorders, and prolonged immobility.
For more information, come into our clinic (close to Remuera, Newmarket and Parnell) to speak to our expert team. It is essential you first get the right diagnosis before any treatment and management occur so book in for a first appointment.

Check out our Online Store for Rehab and Health goods.


A Comprehensive Guide
Living with gluteal tendinopathy (also known as greater trochanteric pain syndrome) can be challenging, but effective treatment options are available. This condition affects the tendons that connect your gluteal muscles to your hip and can cause persistent pain on the outside of your hip.
In this condition, tendons are generally not inflamed, which is why traditional methods like rest and anti-inflammatory medications often don't resolve the issue. Most experts recognize the problem as being degenerative, which may sound intimidating, but it is something that can usually be treated successfully for most people.
To put it simply, the body experiences constant strain from physical activity, leading to wear, and then repairs itself during periods of rest. When the wear occurs faster than the body’s ability to repair, healthy tendons can become weakened and eventually painful.
Several factors influence this wear-and-repair process, such as the intensity of exercise, fitness level, body composition, hormonal shifts, stress, posture, limb alignment, and past injuries. Because of this, simply easing back into activity doesn’t always solve the problem, and a more tailored rehabilitation plan is often necessary. This rehab approach focuses on identifying the specific factors causing the issue and creating an exercise routine to strengthen the gluteal muscles and tendons, improving their ability to tolerate stress.
Tendons have a limited blood supply, meaning that healing and adapting to exercise is a slow process, which is why rehabilitation can take months. However, with consistency and patience, this method typically leads to long-term improvement and successful outcomes.
Key Treatment Approaches:
Prevention Tips:
If you need more information or need help with your hip pain, book a Physio session at Auckland Physiotherapy, Newmarket. If you are unsure who you would like to see, book a complimentary call and talk to one of our expert Physio's today.
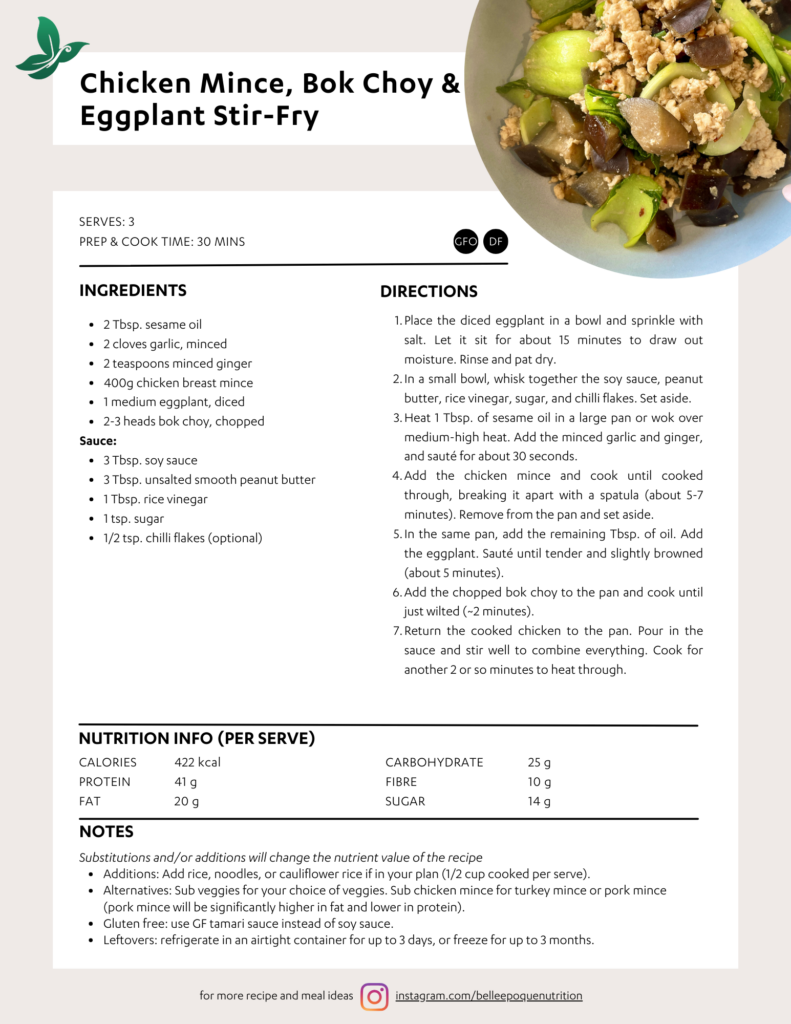
WHAT YOU NEED;
WHAT TO DO;
This recipe was by Karina from cafe delights.
Becoming a mother is one of a woman’s biggest transformations in life, yet we can be so quick to hand over the experience and our trust to others. A care provider may have more knowledge and experience in the world of birth, however they are not qualified in knowing who we are, nor do they have an understanding of our personal foundations - what feels safe to us and what we define as feeling appropriately supported.
Formulating a birth plan can be seen as an exercise that can help you to get clear on what is important to you and can provide you with the clarity to make any decisions that may need to be made during birth feel much less overwhelming.
Why do I need a birth plan?
How do I create a birth plan?
Creating a birth plan is one of the minimal yet most impactful things you can do in preparation for your birth experience and it is never too early to begin.
Your birth plan should be:
Our personal experiences, health and personality will all contribute to how we birth.
There is no one person that can guarantee the birth we may want and we cannot have the chance of having the birth that we want if we do not take accountability to find out what that birth looks like for us.
To help you to get clear on what matters to you for your birth and for support creating your personalised birth plan, book a session with our Maternal Health Consultant, Vanessa Werner.
October is International Breast Cancer Awareness month so I thought I’d take this opportunity to raise awareness on something that many people don’t even realise exists in the cancer treatment space…
Physiotherapy
I’m sure we can all agree that seeing a physio after you’ve had any kind of orthopaedic surgery is almost a given. Similarly if you’re recovering from a neurological injury or illness (brain injury, stroke, Parkinsons) then a physio would probably be on your radar. And even those with respiratory or cardiac conditions will likely have seen a physio at some point.
In cancer treatment it isn’t yet an expected part of someone’s recovery journey. And this needs to change because we can have such a positive impact!
Cancer rehabilitation is a comprehensive treatment approach designed to help a person regain, maintain, or maximise their physical function and emotional wellbeing after a cancer diagnosis. The provision of physiotherapy; including health behaviour change interventions, hands-on treatment, and therapeutic exercise prescription is designed to empower a person back to function and activity. It can be appropriate at any stage of a person’s cancer journey - pre-treatment/surgery, during ongoing treatment and in the recovery and survivorship phases.
In New Zealand, there is currently no routine referral from cancer services to physiotherapy for rehabilitation. This is due to many factors, but ultimately, the current structure is difficult for health care professionals, patients and their whānau to navigate. This results in people with cancer needing to advocate for themselves in order to access cancer rehabilitation services.
The provision of cancer rehabilitation is almost entirely reliant on patient’s being able to pay for treatment themselves or through their insurance. Some financial support can be gained through charitable funding. Fortunately, a substantial number of the major cancer charities in New Zealand currently recognise and support oncology rehabilitation through funding via The Pinc & Steel Cancer Rehabilitation Foundation. Breast Cancer Foundation of New Zealand, Bowel Cancer New Zealand, Talk Peach (gynaecological cancers), Prostate Cancer Foundation and Leukaemia and Blood Cancer Foundation each commit funds to rehabilitation to be delivered by cancer physiotherapists who have undertaken additional, post- qualification, specialised training.
Table 1; below outlines many of the proven benefits of physiotherapy and physical activity on psychological, physical, and social outcomes in cancer. (Image from Physiotherapy in Cancer Care, PNZ 2024)
We know the research supports the involvement of physiotherapists in a person’s cancer journey but it’s also important to hear from those who have experienced it as well. I asked some of our recent clients to share their thoughts on how they came to know about physio, what impact it has had on them and what they would say to anyone who might be considering it:
“I had cording following lymph node removal and I was scared by the possibility of getting lymphedema. I sought out a hospital/community physio who took baseline measurements and gave information, including on The Pinc and Steel Foundation which I followed up. I was pleased to find that I could get funding for further sessions and I'm very grateful for that. I found my physio very easy to talk to. She seemed genuinely interested in me and my welfare. She was knowledgeable and helpful in coming up with short exercise and flexibility programmes that suited the phase of treatment I am in.I have the satisfaction of knowing that I'm doing what I need to for my best recovery. So, for other women, I could say that seeing a cancer rehab physio is a gentle way of actively promoting your own recovery.”
“I came to physio a year after my Breast Cancer diagnosis. I was about 6 weeks post a bilateral mastectomy with reconstruction and my plastic surgeon recommended physio and Pinc and Steel classes. I was keen to start to increase my fitness again after chemo and surgery but I didn’t know where to start. My first visit to physio really highlighted that I needed to get back to basics and learn what my new limits were. I couldn’t even do an abdominal crunch without shaking. This was not only frustrating but eye opening. In subsequent sessions I was able to work on my flexibility and get to know my body better. Pinc and steel classes over 6 week gave me back my confidence and I was able to push myself to do more and more every week. I have felt so supported by my physio all the way. She has been able to develop a program of exercises to suit me and my situation and I don’t think I would be at this same point in my journey without her guidance. I would definitely recommend others seeking out treatment, it’s been an important part in my road to recovery and feeling like ‘me’ again.”
“I was an existing client at AP and found out about the cancer rehab service through my physio. I was looking to improve my overall flexibility and strength, plus build some resilience in my body again. My physio was gentle and measured, her advice was very personalised even though I was in a group class. My mental wellbeing has been the most marked improvement. I would definitely recommend the classes to others - enjoy the expertise, the banter and the supportive atmosphere.”
“My thoughts on the Cancer rehab Physio classes are that anyone offered the opportunity as I was should take it up, if not for the physical benefit which is well worth it but for the fact that they are great fun and it is beneficial to connect with people who have faced the same challenges.”
“After a partial mastectomy and radiotherapy, I had constant pain in my right chest and always sore in my underarm where lymph nodes were removed. I mentioned this to my oncologist on each 6 monthly visit and was told I need to learn to live with it. Sadly, at no stage was I ever offered or advised there was any help out there until one of the physios at AP mentioned the option of their cancer rehab service. My goal was to learn how to manage the pain, gain strength in my arm and be able to get more movement given it is my dominant arm. I was happy to try anything.I also became aware that it had affected my breathing considerably. Chest breathing had become a habit as a protection measure for pain.
Everyone I came into contact with to get set up for the programme were incredibly helpful and positive which was so encouraging and positive for your mental health. You were not alone.I am beyond grateful to be a part of this group. My personal journey has been mind blowing. The specialised exercises have given me a new lease on life, not only has the pain in my arm and chest improved 100% I have been given the tools to learn how to breathe more efficiently. It has given me so much confidence in my daily life.”
Hearing this from our clients makes me extremely proud of the cancer rehabilitation we can provide at AP. Our service is appropriate for anyone with a cancer diagnosis and at any stage in their journey. We have a range of 1-1 or group class options available and are able to link you up with the appropriate charities if you require financial assistance.
If you’d like to find out more you can read about the service on our website or book a complimentary cancer rehab information call with Kirsten to discuss your needs.
If you’d like to support someone you know or make a donation to The Pinc and Steel Foundation you can do so here
By Kirsten Rose, Physiotherapist & Health Coach.
This was the theme for Mental Health Awareness Week this year. It reminds us of the importance of social support and connection with others in order to foster not only our mental wellbeing, but our wellbeing as a whole. As a species, humans are wired for connection but in this modern age, despite the hyperconnectivity that technology allows, many people still feel lonely and isolated.
I was at a conference recently and one of the speakers presented on the theme that physical activity is like social glue. He talked about how we feel about exercise being more important than what we think about it (and hence the reason why just because we know it’s good for us doesn’t always translate into doing it!). We need to feel positively connected to that exercise to give us a compelling reason to do it. There is also mounting research that shows that people coming together to be active ramps up the benefits to their wellbeing, far exceeding the benefits of the exercise itself, and hence giving us that compelling reason to do it! For those of you who know me from the clinic, you’ll understand when I say I was just fizzing about this topic.
On a personal level this resonates so deeply with me. Team sports have been a huge part of my life since I was a kid. As an adult, Crossfit has truly been my social glue for the past decade. Being a part of that community has helped me ride through many a storm - moving back to Auckland after many years away, helping me to maintain both my physical and mental health through the wild ride of becoming a parent, those ridiculous covid years, and all the other curveballs that life regularly throws at our way. Yes I love it as a form of exercise, but it’s the people that make it extra special and have helped me to stay consistent over all this time. I’d also say that over the years I’ve recognised it’s importance for my mental health and fitness, not just for the physical or aesthetic gains.
Amongst the team here at AP, it’s a common theme. Whether it’s running, triathlons, multisport, pilates, yoga, tramping, dancing, team sports…we all value the social connection and headspace that our chosen form of exercise gives us. It’s why we can relate to our clients when pain, illness or injury gets in the way of taking part in these activities. Because it’s not just exercise buzz that we miss is it?
What we miss is something that’s called “collective effervescence” - the energy that comes from being in a group with a shared purpose. The feeling that you get from the supportive scaffolding that those people provide, so even on a bad day, you know you can turn up and 99% of the time leave feeling so much better!
So what do you do when you can’t be part of your chosen community for a while?
Especially if you notice that you’re starting to feel the negative mental effects of less regular exercise and social connection then we need to be proactive…
Firstly let’s talk about that word “can’t” cos as humans we’re pretty good at black and white thinking. I know I’m not alone with the “if I can’t do it in the way that I want then I won’t do it at all” story. Yep I see you nodding as you read this. Is there another version of that story that might actually be more true? Perhaps a reframe like this might be more helpful… “I could go and I’ll be slower/need to ask for help/have to modify a few things but I could still be there”.
If you really can’t do it then there’s two things we need to consider:
Firstly, you’re allowed to feel like that sucks, make some room for those emotions. Being unwell and/or injured often isn’t fun. It can be frustrating, stressful and for sure it can rob you of some of the joys of life for a while. You don’t need to pretend like that’s not happening. However, ruminating and getting stuck in those negative thought loops isn’t helpful so onto the next consideration…
What are the opportunities that this injury/illness might be providing you? Not in a toxic positivity way, but in a realistic and optimistic way, as there is often room for growth in times of adversity.
Maybe if your injury is only in one part of your body, you can focus your training elsewhere to tidy up that technique or strength difference you’ve been meaning to address for ages. Maybe there’s now time available to learn something new - for many of us exercise is our best tool to manage stress, but could this be a chance to learn more about what breathwork, mindfulness or a creative pursuit could do for your stress as well?
Here at AP, we‘re passionate about ensuring that our clients can be supported along their whole recovery journey. We can be your community when you need us.
That might look like starting with one of our physiotherapists and progressing to one of our physio-led group classes to get you back on track, then working with our Health Collective team of pilates instructors, personal trainers and massage therapists to keep you well. And there’s the option of Health Coaching anywhere along that journey to support you with making those mindset shifts so your new routines and habits are both successful and sustainable.
I’d like to leave you with this wonderful quote from Vivek Murthy, the US Surgeon General…
“We succeed and thrive best when we work together and support each other.
When we struggle alone, that’s when the struggle can seem impossible”
So don’t go it alone. Reach out and let us help you. We’re experts in making better lives possible.
If you would like to learn more click on our Health Coaching page or book a complimentary call with Kirsten HERE.